FAQ
I have a STROKE - what shall I do?
Call the Emergency Services immediately!
112 from any European Mobile Phone, use the emergency dial button
18 for Monaco Firefighters (Ambulances), 17 for Emergency Services
The Stroke center for Monaco is the CHU in Nice
Hospital Pasteur - Hôpital Pasteur, 30 Voie Romaine, 06000 Nice (France)
Tel: +33 4 92 03 77 77
The CHPU Monaco doesn't have a stroke unit, see article February 2023:
https://monaco-hebdo.com/actualites/sante/benoite-rousseau-de-sevelinges-interview-chpg-attractivite-2023/
112 from any European Mobile Phone, use the emergency dial button
18 for Monaco Firefighters (Ambulances), 17 for Emergency Services
The Stroke center for Monaco is the CHU in Nice
Hospital Pasteur - Hôpital Pasteur, 30 Voie Romaine, 06000 Nice (France)
Tel: +33 4 92 03 77 77
The CHPU Monaco doesn't have a stroke unit, see article February 2023:
https://monaco-hebdo.com/actualites/sante/benoite-rousseau-de-sevelinges-interview-chpg-attractivite-2023/
What type of strokes exist?
- Ischaemic Strokes are caused by a blockage cutting off the blood supply to the brain. (The most common).
- Haemorrhagic Strokes are caused by a bleeding in or around the brain.
- TIAs - Transient Ischaemic Attacks known as a mini-strokes. A TIA is the same as a stroke, except that the symptoms only last for a short amount of time. This is because the blockage that stops the blood getting to your brain is temporary. It is uttermost important to recognize those and get treatment, as there is a high risk of having a regular stroke afterwards.
How do I recognize a stroke with the FAST test?
- Face dropping
- Can the person smile?
- Did the eye or mouth dropped or look different?
- Arm weakness
- Can the person raise both arms? Move the legs, hands, feet?
- Sudden weakness or numbness of the body is a sign of a stroke
- Speech problems
- Can the person speak clearly? And understand what you say?
- Difficulty speaking or "no words come out" is a sign of stroke
- Time to call emergency 112

Stroke is a medical emergency!
The FAST test can help you recognise a stroke, further signs are:
- A sudden, severe headache, often with real pain
- Sudden memory loss or confusion
- Blurred vision or loss of sight in one or both eyes
- Dizziness or a sudden fall
Hospital Pasteur - Hôpital Pasteur, 30 Voie Romaine, 06000 Nice Tel: +33 4 92 03 77 77
Can you recover from stroke?
All patients have a different history, and all strokes are different.
Some people may have relatively minor effects and those may not last long. Others may be left with more serious problems, need short or long term therapy or will even stay with disabilities that make them dependent on other people.
Unfortunately, some strokes can be very serious and some may lead to coma or sudden death. That’s why it’s so important to be able to recognise the symptoms and get medical help as quickly as possible.
The quicker you receive treatment, the better your chances for a good recovery.
Read more:
https://www.stroke.org.uk/what-is-stroke/types-of-stroke
Some people may have relatively minor effects and those may not last long. Others may be left with more serious problems, need short or long term therapy or will even stay with disabilities that make them dependent on other people.
Unfortunately, some strokes can be very serious and some may lead to coma or sudden death. That’s why it’s so important to be able to recognise the symptoms and get medical help as quickly as possible.
The quicker you receive treatment, the better your chances for a good recovery.
Read more:
https://www.stroke.org.uk/what-is-stroke/types-of-stroke
What causes stroke?
When the blood supply to part of the brain is blocked or reduced, an ischemic stroke occurs.
When a blood vessel in the brain leaks or bursts and causes bleeding in the brain, a hemorrhagic stroke occurs.
A stroke is a medical emergency. Getting medical help quickly!
https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
When a blood vessel in the brain leaks or bursts and causes bleeding in the brain, a hemorrhagic stroke occurs.
A stroke is a medical emergency. Getting medical help quickly!
https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
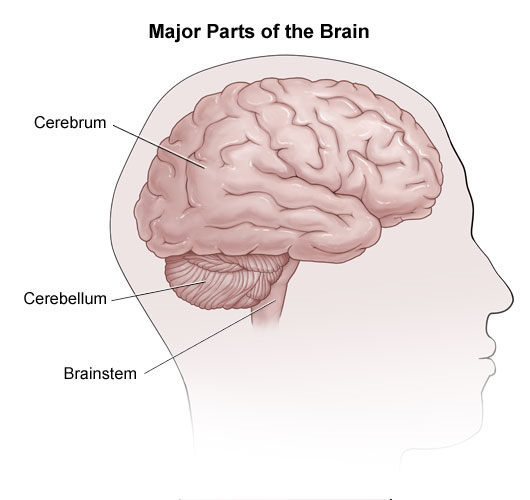
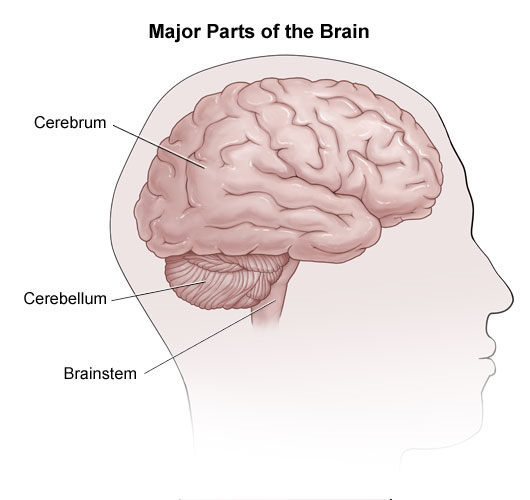
Where in the Brain does the Stroke occur?
The brain is divided into 3 main areas, depending on where the Stroke is, it may have different effects as also each patient is different. Main brain areas are:
 https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
- Cerebrum (right and left sides or hemispheres)
- Cerebellum (top and front of the brain)
- Brainstem (base of the brain)
 https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-strokeWhat are the effects of a stroke?
Effects may be:
- Difficulty with movement or paralysis
- Sensory and physical impairments, or inability to localize or recognize body parts
- Problems with coordination and balance (ataxia)
- Chewing, swallowing, speech and language
- Eating and swallowing, bowel and bladder control
- Memory and Cognitive issues (thinking, reasoning, judgment), inability to find objects, or locations
- Headache, Dizziness, Nausea and vomiting
- Visual problems, and spatial problems with depth perception or directions
- Emotional and behavioral changes, such as lack of concern about situations, impulsivity, inappropriateness, depression, or denial ("neglect")
- Sexual ability
- Breathing and heart functions
- Body temperature control
How can I prevent a stroke?
Among age, and we all get older, certain medical conditions can increase your risk of stroke. Having them checked and eventually adjusting your lifestyle can help you preventing a stroke:
Check also your family history, if a close relative (parent, grandparent, brother or sister) has had a stroke. Speak to your General Practitioner if you have close relatives with stroke or heart attack, as some kinds of high cholesterol can run in families.
- High blood pressure is the single biggest risk factor for stroke. Check your blood pressure regularily
- Atrial fibrillation can lead to a clot forming in your heart, causing a stroke. If you feel heart arrythmia, speak with your doctor.
- High cholesterol and Diabetes are further risk factors.
Check also your family history, if a close relative (parent, grandparent, brother or sister) has had a stroke. Speak to your General Practitioner if you have close relatives with stroke or heart attack, as some kinds of high cholesterol can run in families.
Stroke Risk Factors
Risk Factors that you can control account for 82% to 90% of all strokes:
Further risk factors are based on lifestyle, genetic , and environment.
- High blood pressure
- Obesity / Physical inactivity
- Poor diet / Diabetes / High Blood Cholestorol
- Smoking
Further risk factors are based on lifestyle, genetic , and environment.
- Age is a risk factor, too. A stroke can occur at any age, but the risk is higher for babies under the age of 1 and for adults as they grow older.
- Anxiety, depression, and high stress levels, as well as working long hours and not having much contact with family, friends, or others outside the home, may raise your risk for stroke.
- Family history and genetic play a role as well. Your risk of having a stroke is higher if a parent or other family member has had a stroke, particularly at a younger age. Certain genes affect your stroke risk, including those that determine your blood type. People with blood type AB (which is not common) have a higher risk.
- Living or working in areas with air pollution can also contribute to stroke risk.
- Other medical conditions, such as sleep apnea, kidney disease, and migraine headaches, are also factors.
- Other unhealthy lifestyle habits, including drinking too much alcohol, getting too much sleep (more than 9 hours), and using illegal drugs such as cocaine, may raise stroke risk.
- Sex can play a role in risk for stroke. At younger ages, men are more likely than women to have a stroke. But women tend to live longer, so their lifetime risk of having a stroke is higher. Women who take birth control pills or use hormone replacement therapy are at higher risk. Women are also at higher risk during pregnancy and in the weeks after giving birth. High blood pressure during pregnancy — such as from preeclampsia — raises the risk of stroke later in life.
- Viral infections or conditions, such as lupus or rheumatoid arthritis, can cause inflammation.
What therapies are available for post-stroke treatment?
Therapy will depend on each patient's situation, and the rehabilitation plan will change during the recovery process, depending on which part(s) of the body or abilities were affected and the type and severity of damage.
However let's have a look at certain stroke rehabilitation therapies and the variety of specialists involved:
1. Physical Therapy
2. Occupational Therapy is a more task-focused type of training, and therapists work with stroke survivors on practical, real-world, day-to-day tasks such as getting in and out of bed and dressed, eating & drinking, and general walking and climbing of stairs. Occupational therapists also help to improve sensory abilities while ensuring safety in the post-stroke period, such as for personal grooming, preparing meals, and housecleaning.
3. Speech and Swallow Therapy will support you in getting
those skills back, as they require thinking about the action while coordinating muscles of the face, mouth, tongue, and throat. Speech-language pathologists help a person relearn how to use language or develop alternative means of communication, and they also might teach problem-solving and social skills needed to cope with those aftereffects of a stroke. Speech therapy can be focused on understanding words as well as on producing words that others can clearly understand, and usually involves longer practice and repetition. Swallowing problems are usually more of an unpleasant surprise, but can be life threatening, and therapie to improve swallowing starts typically directly in the hospital, eventually by learning the "chin-tuck maneuver" : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4687995/
4. Visual Therapy and balance therapy are often scheduled in combined rehabilitation sessions for stroke survivors, because vision partially relies on good balance and balance partially relies on good vision, and the areas of the brain that control these two functions have to interact.
5. Cognitive Therapy involves interventions that are designed to improve thinking skills and problem-solving abilities, such as using computer-generated and video-game rehabilitation therapy. Stroke survivors who participate in cognitive therapy recover better than stroke survivors who do not. Stroke survivors recovering from a cortical stroke often have more cognitive issues than after recovering from a small vessel subcortical stroke, and left-sided cortical strokes cause different cognitive deficits than right-sided ones.
6. Innovative Physical & New Types of Therapy are including mirror therapy, and electrical therapy, biological therapy, and alternative medicine includes treatments such as massage, yoga, meditation, herbal therapy, acupuncture, music and oxygen therapy. New therapies include Noninvasive brain stimulation, and techniques such as transcranial magnetic stimulation which have been used with some success in a research setting to help improve a variety of motor skills. Biological therapies, such as stem cells, are being investigated, but should only be used as part of a clinical trial. , where results are being evaluated. Research studies show that the use of new and innovative rehabilitative therapies tend to test better on measures of stroke outcomes and usually do not experience negative effects.
7. Psychatrical and Psychological Therapy: Psychologists, and Psychatrists can help with the person’s mental and emotional health and assess cognitive skills, as well as support stress, e.g. with EDMR.
8. Doctors, Physicians & Nurses: Your doctors have the primary responsibility for managing and coordinating the long-term care of you as a stroke survivor, including recommending which rehabilitation programs will best address your individual needs. However, with our experience we like to encourage you to take an active part in this. Doctors supporting often include physiatrists (specialists in physical medicine and rehabilitation), neurologists, internists, geriatricians (specialists in seniors), and family practice physicians. A physician also may recommend medicines to ease pain or treat a condition. Specialized rehabilitation nurses can help a stroke victim relearn the skills needed to carry out the basic activities of daily living. They also provide information about routine health care, such as how to follow a medication schedule, how to care for the skin and manage bladder and bowel issues, how to move out of a bed and into a wheelchair, and special needs for people with diabetes.
9. Job Consultants or Vocational Therapists may support in career counsel, and in helping you in case of residual disabilities to identify vocational strengths and develop résumés that highlight those strengths. They also can help to identify potential employers, assist in specific job searches, and provide referrals to vocational rehabilitation agencies. Usually they work hand in hand with social workers, who can assist with making financial decisions and plan the return home or to a new living place. They also can help plan for care after being discharged from a rehabilitation facility.
https://www.mayoclinic.org/diseases-conditions/stroke/in-depth/stroke-rehabilitation/art-20045172
https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Stroke-Rehabilitation-Fact-Sheet#whatis
https://www.youtube.com/watch?v=2lMtwbj5TTc
However let's have a look at certain stroke rehabilitation therapies and the variety of specialists involved:
1. Physical Therapy
2. Occupational Therapy is a more task-focused type of training, and therapists work with stroke survivors on practical, real-world, day-to-day tasks such as getting in and out of bed and dressed, eating & drinking, and general walking and climbing of stairs. Occupational therapists also help to improve sensory abilities while ensuring safety in the post-stroke period, such as for personal grooming, preparing meals, and housecleaning.
3. Speech and Swallow Therapy will support you in getting
those skills back, as they require thinking about the action while coordinating muscles of the face, mouth, tongue, and throat. Speech-language pathologists help a person relearn how to use language or develop alternative means of communication, and they also might teach problem-solving and social skills needed to cope with those aftereffects of a stroke. Speech therapy can be focused on understanding words as well as on producing words that others can clearly understand, and usually involves longer practice and repetition. Swallowing problems are usually more of an unpleasant surprise, but can be life threatening, and therapie to improve swallowing starts typically directly in the hospital, eventually by learning the "chin-tuck maneuver" : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4687995/
4. Visual Therapy and balance therapy are often scheduled in combined rehabilitation sessions for stroke survivors, because vision partially relies on good balance and balance partially relies on good vision, and the areas of the brain that control these two functions have to interact.
5. Cognitive Therapy involves interventions that are designed to improve thinking skills and problem-solving abilities, such as using computer-generated and video-game rehabilitation therapy. Stroke survivors who participate in cognitive therapy recover better than stroke survivors who do not. Stroke survivors recovering from a cortical stroke often have more cognitive issues than after recovering from a small vessel subcortical stroke, and left-sided cortical strokes cause different cognitive deficits than right-sided ones.
6. Innovative Physical & New Types of Therapy are including mirror therapy, and electrical therapy, biological therapy, and alternative medicine includes treatments such as massage, yoga, meditation, herbal therapy, acupuncture, music and oxygen therapy. New therapies include Noninvasive brain stimulation, and techniques such as transcranial magnetic stimulation which have been used with some success in a research setting to help improve a variety of motor skills. Biological therapies, such as stem cells, are being investigated, but should only be used as part of a clinical trial. , where results are being evaluated. Research studies show that the use of new and innovative rehabilitative therapies tend to test better on measures of stroke outcomes and usually do not experience negative effects.
7. Psychatrical and Psychological Therapy: Psychologists, and Psychatrists can help with the person’s mental and emotional health and assess cognitive skills, as well as support stress, e.g. with EDMR.
8. Doctors, Physicians & Nurses: Your doctors have the primary responsibility for managing and coordinating the long-term care of you as a stroke survivor, including recommending which rehabilitation programs will best address your individual needs. However, with our experience we like to encourage you to take an active part in this. Doctors supporting often include physiatrists (specialists in physical medicine and rehabilitation), neurologists, internists, geriatricians (specialists in seniors), and family practice physicians. A physician also may recommend medicines to ease pain or treat a condition. Specialized rehabilitation nurses can help a stroke victim relearn the skills needed to carry out the basic activities of daily living. They also provide information about routine health care, such as how to follow a medication schedule, how to care for the skin and manage bladder and bowel issues, how to move out of a bed and into a wheelchair, and special needs for people with diabetes.
9. Job Consultants or Vocational Therapists may support in career counsel, and in helping you in case of residual disabilities to identify vocational strengths and develop résumés that highlight those strengths. They also can help to identify potential employers, assist in specific job searches, and provide referrals to vocational rehabilitation agencies. Usually they work hand in hand with social workers, who can assist with making financial decisions and plan the return home or to a new living place. They also can help plan for care after being discharged from a rehabilitation facility.
https://www.mayoclinic.org/diseases-conditions/stroke/in-depth/stroke-rehabilitation/art-20045172
https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Stroke-Rehabilitation-Fact-Sheet#whatis
https://www.youtube.com/watch?v=2lMtwbj5TTc
What is Physical Therapy (Physiotherapy)
Physical Therapy includes a variety of muscle maneuvers, activities and exercises designed to train the brain and the muscles to work together.
It uses an approach that builds muscle strength and maintains healthy muscle tone. Nearly any 30-60 min 5-7 days/week physical therapy is effective to improve your mobility, walk at a faster pace, function more independently, and have a better balance, and is usually already initiated in the hospital, shortly after the stroke.
Your physical therapist should be specialized in treating disabilities related to motor and sensory impairments, and be able to help restore physical functioning by evaluating and treating problems with movement, balance, and coordination; and constraint-induced therapy, in which an unaffected limb is immobilized, causing the person to use the affected limb to regain movement and function, but also independence, and quality of life.
Picture: Courtesy to Steven Saltzman, the pictures shows him with his private coach.
It uses an approach that builds muscle strength and maintains healthy muscle tone. Nearly any 30-60 min 5-7 days/week physical therapy is effective to improve your mobility, walk at a faster pace, function more independently, and have a better balance, and is usually already initiated in the hospital, shortly after the stroke.
Your physical therapist should be specialized in treating disabilities related to motor and sensory impairments, and be able to help restore physical functioning by evaluating and treating problems with movement, balance, and coordination; and constraint-induced therapy, in which an unaffected limb is immobilized, causing the person to use the affected limb to regain movement and function, but also independence, and quality of life.
Picture: Courtesy to Steven Saltzman, the pictures shows him with his private coach.


